It is not always clear what causes malabsorption, but it can be devastating because our body has no proper functioning of the nutrients. Malabsorption is more common in many chronic diseases, and many patients need supplementation in some form or another.
In this article, we’ll look at what malabsorption is, why it happens, how it affects our bodies, and what we can do to prevent nutrient deficiencies.
What is Malabsorption?
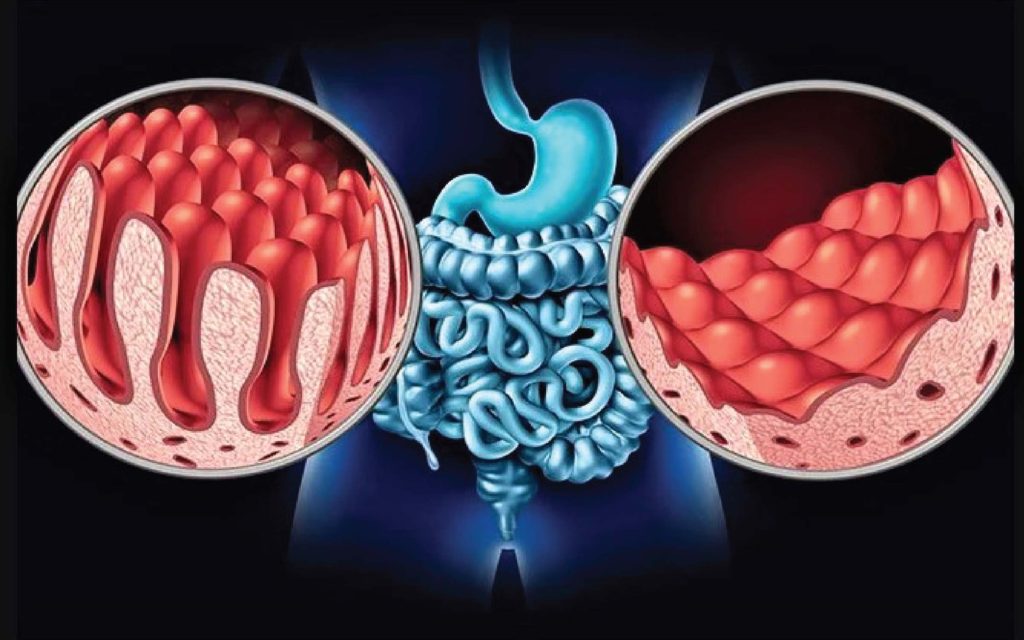
It refers to a number of disorders in which nutrients from food are not absorbed properly in the small intestine.
Usually, macronutrients and micronutrients are break down in the small intestine when we are eating food. Then the body absorbs them in the bloodstream.
This is disrupted if the body cannot digest or absorb these nutrients, if malabsorption happens. Autoimmune disease, operation, infection, congenital defects or genetic defects are causes.
Causes of Malnutrition in Chronic Illness Patients
Some chronic diseases, such as: Irritable Bowel, IBS, Crohn’s Disease, Ulcerative Colitis, Celiac Disease, and Mast Cell Activation Syndrome (MCAS), and Short Bowel, are particularly sensitive to malabsorption (SBS).
The cell linings may be inflamed, destroyed or nonresponsive in these diseases or disorders. Small inflammation of the intestines can lead to food digestion and nutrient absorption problems. Widespread inflammation of the intestines (including the colon and rectum) can cause water and electrolyte absorption problems.
In IBD patients, inflammation occurs in the gut that can lead to bowel surface ulceration. In turn, this results in chronic blood malabsorption and protein loss.
In addition, patients cannot eat because of the symptoms of nausea, vomiting, diarrhea and abdominal pain. You can also have limited options for food. The food shortage and consequently the consumption of nutrients plays an essential role in malnutrition.
There is evidence that a large proportion of inflammatory bowel disease (IBDs) patients are affected by malnutrition,’ which is estimated in 65%-75% of Crohn’s disease patients (CDs) and in 18%-62% of UCs.
The cell linings may be inflamed, destroyed or nonresponsive in these diseases or disorders. Small inflammation of the intestines can lead to food digestion and nutrient absorption problems. Widespread inflammation of the intestines (including the colon and rectum) can cause water and electrolyte absorption problems.
In IBD patients, inflammation occurs in the gut that can lead to bowel surface ulceration. In turn, this results in chronic blood malabsorption and protein loss.
In addition, patients cannot eat because of the symptoms of nausea, vomiting, diarrhea and abdominal pain. You can also have limited options for food. The food shortage and consequently the consumption of nutrients plays an essential role in malnutrition.
Drugs as a malabsorption factor
Drugs used in control and chronic disease management can also cause malabsorption. Malabsorption. Glucocorticosteroids are known to interfere with calcium absorption, for example. Osteoporosis and other health issues can result. In fact, the most frequent bone disease is osteoporosis, until a broken fracture occurs.
Sulfasalazine is a DMARD (disease-modifying anti-rheumatic drug) that doctors sometimes use in patients with UC or IBD. It is also a folic antagonist. The aim is to control and treat bowel inflammation, diarrhea, rectal bleeding and abdominal pain. Side effects, ironically, can mirror the symptoms of the disease.
Some impacts from malabsorption
A wide range of symptoms can occur depending on the type of nutrient loss or malabsorption, for example:
- Anemia
- Chronic fatigue
- Sleeping disorders
- Female infertility
- Osteoporosis or osteopenia
- Hypertension
- Cardiomyopathy
- Poor wound healing
- Night blindness
In IBD patients, certain common vitamin and nutrient shortcomings include:
- Iron
- Calcium
- Selenium
- Zinc
- Magnesium
- Vitamins (especially vitamin A, B12, Folic Acid, D and K)
Surgery & Malnutrition in IBD Patients
In the first ten years after diagnosis, up to 50 percent of Crohn’s patients need to have surgery. In addition, up to 85 percent of patients awaiting surgery are malnourished.
Worse, malnourishment can have an effect on the surgical outcome. This is especially true for those suffering from chronic diseases, who are already predisposed to other risk factors and have a weakened immune system.
In IBD patients, malnutrition rates range between 25 – 69%. It can affect every part of the gastrointestinal tract and is especially common in Crohn’s disorder. Compare this to UC, which is limited to colon inflammation.
The growth of obesity and the need for bariatric operation
In modern society, morbid obesity is another major problem. The numbers are rising in the next few years and will reach nearly one million. In this population there are common nutritional deficiencies like vitamin B12 and iron.
There are over 100,000 annual bariatric (weight loss) operations. This operation alters the digestive system’s anatomy. These changes mean the body no longer has the time or space to break down food ‘as usual’ for absorption and use. Other health problems such as metabolic problems and ulcers may be accompanied by malnutrition.
In general, in two-thirds of these patients within 4 years of surgery, fat-soluble vitamins A, D and K are poor. This results in other health issues such as easy flushes, rashes, osteocalcin and more depending on the type of food deficiency.
Bacterial Overgrowth (SIBO)’s Impact on Malabsorption
SIBO (small intestinal bacterial overgrowth) is a common cause of malabsorption. While probiotics tend to be good for intestinal flora, there are some that contain prebiotics like fructooligosaccharides or inulin. These carbohydrates feed intestinal bacteria. But overcrowding and worsening gastrointestinal (GI) symptoms can also occur.
Intestinal hyperpermeability (aka leaky intestine) and SIBO are common symptoms for people who have a strict gluten-free diet with celiac disease.
Antibiosis that kills or disturbs intestinal flora and narcotics can slow down intestinal transit also form other acute causes of SIBO (motility). SIBO is also a transient cause of rotaviruses, astroviruses and noroviruses.
Intestinal bacteria also like iron and sometimes absorb it, which leads to iron deficiency before the body can use it.
Microbial Infections That Can Cause Malabsorption
Infections by Protozoa and Helminths, and intestinal tuberculosis and chronic pancreatitis can also cause malabsorption. These occur particularly in the tropics and are called “tropical malabsorption.” IBD and Celiac disease have also increased in tropics leading to malabsorption.
Final remarks
Malabsorption is a complex subject, which is often not taken into account. Even by medical professionals, it is often not collected early enough. The effect on the patient may be harmful. The effects of malabsorption are sometimes not easily evident and further testing is necessary.
There are many root causes that can lead to malabsorption, as detailed above. No matter what the cause, nutrients are essential to replenish the body. They are important in every person for optimum health and well-being.